Beyond Mandatory Autonomy: Rethinking Decision-Making in Serious Illness

The Autonomy Myth and Why It’s Failing Us
Truth bomb: “Do you want us to shock his heart if it stops?” is not a neutral question. It’s a transfer of burden dressed up as respect.
TL;DR
We over‑valorize autonomy and confuse neutrality with respect. Those of us in this culture and on this side of the world think of each human as sealed within a solo chamber of autonomy, devoid of influence from their loved ones and community (hint: there are better ways).
In the hospital, that habit breeds learned helplessness, decision paralysis, and non‑beneficial care. Shared decision‑making on Kon’s continuum—where clinicians offer values‑based recommendations and invite dissent—performs better ethically and clinically. Use the playbook below to get there.
How we got here (and why it’s not working)
Autonomy emerged as a necessary correction to old-school paternalism, anchored in informed consent and rights. But the modern reflex—“it’s your choice”—often devolves into abandonment‑by‑neutrality when decisions are complex and time‑pressured. Patients want agency; they also need expert guidance calibrated to their values. For physicians, knowledge without a sense agency leads to moral distress.
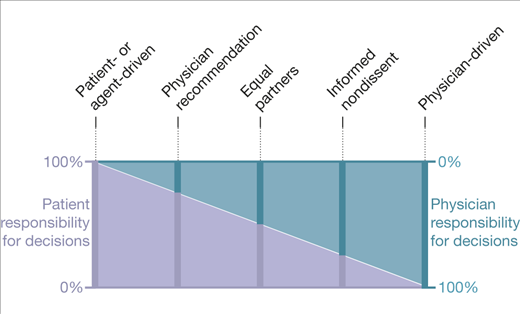
Critical care and pediatric societies now endorse shared decision‑making (SDM), explicitly including clinician recommendations rooted in the patient’s values, not the clinician’s preferences. Kon’s continuum offers a practical dial—from patient‑driven to physician‑driven—with multiple shared variants in between. It replaces moral absolutism with context‑sensitive deliberation.
The fallout of “mandatory autonomy”
Three predictable pathologies show up when we make individualistic autonomy the only star:
- Learned helplessness among families: about half of ICU surrogates meet criteria for learned helplessness; risk rises with stress and lower education, and drops when an advance directive or DNR exists. Translation: neutral menus in crises impair decision quality.
- Decision paralysis: indecision drives delays and more aggressive care later. Recognizing and defusing paralysis requires structured approaches that most teams lack.
- Non‑beneficial care creep: ICU interventions aiming at better surrogate decision‑making reduce length of stay among dying patients without changing mortality. Better conversations, fewer protracted non‑beneficial stays.
Two moments you’ve lived
- The burden‑shift: Night admit, refractory shock. The team offers “full code vs DNR,” framing CPR as a family choice. The daughter asks, “What would you do?” The neutral pose feels respectful yet abandons the family to a moral cabinet full of empty shelves.
- The values‑anchored pivot: Same physiology, different script: “Given his priorities—avoiding machines and being home—CPR won’t help him reach those ends. I recommend we focus on comfort and avoid CPR. If that doesn’t feel right, please say so.” Distress drops; choices align with goals.
Kon’s continuum: set the dial, don’t worship a pole
The shared decision‑making continuum formalizes five workable stances:
- Patient‑driven (relational autonomy) for clearly value‑laden choices the patient wants to own.
- Equal partnership for complex trade‑offs with uncertainty.
- Physician recommendation when values are known and the patient explicitly invites guidance.
- Informed non‑dissent (or assent) when an option is non‑beneficial; you state the plan and invite objection.
- Physician‑driven generally only for truly value‑neutral technical decisions, while staying alert to hidden preferences.
"Listen, Kyle, I need a picture"
Done and done.
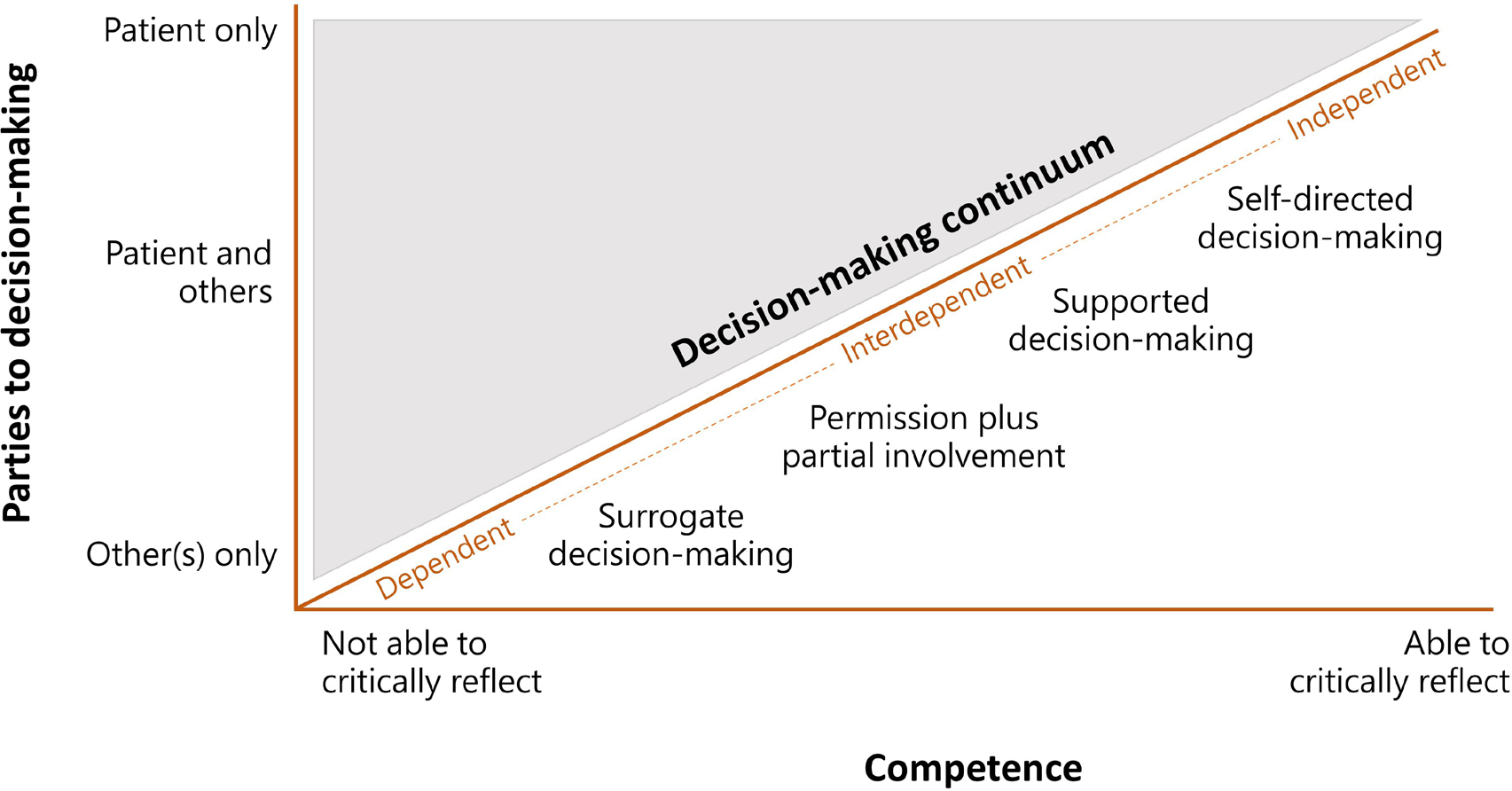
But let's dial it up one more notch and remember that everyone exists in relational community:
Building the Playbook (usable tomorrow)
1) Map values + hope style
Ask verbatim: “What matters most if time is short?” Document exact words. Then tag the dominant hope approach: Technical (more treatment), Spiritual (meaning/faith), Minimalist (comfort, less intervention), Pragmatic (time at home, function). Early, structured goals‑of‑care conversations improve alignment, family outcomes, and reduce non‑beneficial care near death.
2) Set the Kon dial
Offer a stance choice: recommendation vs equal partnership vs non‑dissent for non‑beneficial options. Say it out loud: “Some people want my recommendation; others want to decide together.” Make explicit that any recommendation reflects the patient’s values, not yours.
3) Build awareness iteratively
Use Ask‑Tell‑Ask: assess understanding → share tailored info → check back. Pair Hope/Worry/Wonder: “I hope for more time; I worry CPR won’t help you leave the hospital; I wonder if we can focus on comfort and home.” Document current prognostic awareness and expect “middle knowledge” (oscillation between hope and realism).
4) Check bias/power
Name mistrust, language needs, and your positional power. Invite correction: “If I miss or misinterpret something, please stop me.” SDM struggles in the hospital include uncertainty, time pressure, fear of losing control; surface them so you can manage them.
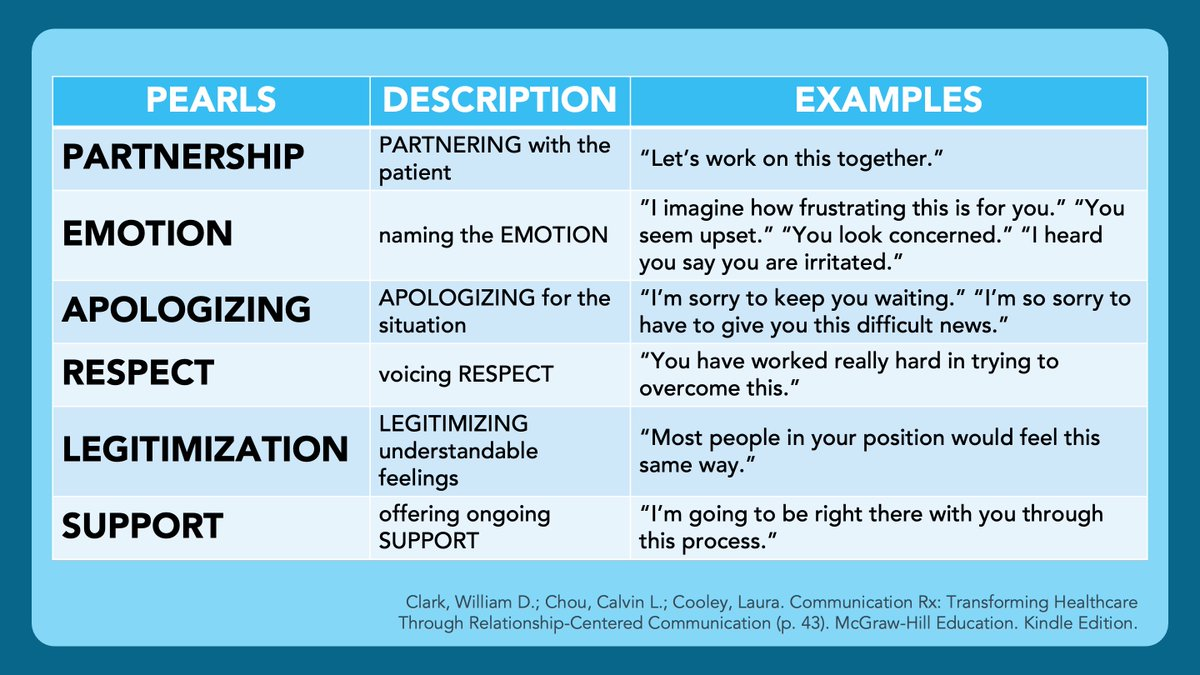
5) Pivot when flooded
If open‑ended questions backfire, switch to structured clarity: short declaratives, explicit compassion, and focused options only. Use PEARLS skills (never NURSE, that acronym is terrible) alongside Ask‑Tell‑Ask to regulate emotional bandwidth.
6) Highlight the best choice (the maternalistic move)
When trust is strong, values are known, and the patient wants guidance, present a package deal aligned with goals with an off‑ramp to dissent: “Given what matters to you, my recommendation is no CPR, comfort‑focused care, and discharge home with hospice. If that feels wrong, say so and we’ll adjust.”
This is recommendation inside SDM, not coercion.
7) Use informed non‑dissent for non‑beneficial CPR
Elicit values → explain why CPR won’t achieve those ends → state a caring assessment → invite disagreement. Trials are testing this approach among older, seriously ill adults, and ethical analyses support its use. Local law/policy varies; know your institution’s stance.
8) Align orders with goals
Stop offering interventions that cannot reach the patient’s stated ends. Replace checkbox code talks with values‑anchored care plans.
Why nuance beats purity
Autonomy alone can’t carry the weight in crisis. Deliberative SDM on Kon’s continuum respects agency and leverages expertise. It also mitigates psychological harms (helplessness, paralysis) and curbs non‑beneficial care when outcomes cannot match goals.
Script you can use on rounds today
Open: “What matters most if time is short?”
Translate: “Given that, here’s my recommendation.”
Invite dissent: “If it doesn’t fit, please say so and we’ll adjust.”
Align orders to goals. No menu without meaning.
Next up in this series
Part 2 — A deep dive on Maternalism and the Ethics of Clinician-Guided Care





