Compassion on Clearance: Why Palliative Values Always Seem to End Up Out of Stock
If you’ve ever wondered why working in healthcare, especially in Specialist Palliative Care, feels like its being pulverized by grinding gears, this essay is for you.

Every memo says patients come first. Every town hall promises dignity and whole-person care. And yet we're all staring at a dashboard that cares more about RVUs than humanity. If you’ve ever wondered why working in healthcare, especially in Specialist Palliative Care, feels like its being pulverized by grinding gears, this essay is for you.
Context
My team has recently experienced some changes that have made us all feel like the quality of palliative care we provide has been degraded and the productions pressures have been ramped-up. And yet this seems in direct contradiction to the values espoused by leadership. I am a visual person and I have been describing this phenomenon as the values being "ground up" in layers of gears between what comes out of our most visionary health system leaders' mouths and what becomes of those words once they emerge from the middle management layer. This essay reflects my analysis of the systems at play.
The Big Picture
Healthcare speaks the language of compassion but runs on a logic of margin. This is not accidental—it is structural.
The U.S. health care system was rebuilt on market principles. Corporatization, commercialization, and financialization have reshaped priorities.
What begins as a vision of dignity and whole-person care is translated into dashboards, RVUs, and compliance metrics. Each layer strips away relational values until, at the bedside, clinicians face quotas instead of conversations.
This dynamic explains why moral injury is rising. Clinicians know what good care looks like but are constrained by systems optimized for throughput. Burnout is not a personal failing; it is the predictable outcome of a design that prizes solvency over solidarity.
Palliative care exposes the contradiction most clearly. Its benefits—comfort, meaning-making, family healing—are real, but economically illegible. The same forces that claim to value compassion apply metrics that undermine it. When your worth is measured in consult counts, the soul of the work evaporates.
But this is not unique to palliative care. Across the U.S., relational work—teaching, social work, childcare, nursing—shares a common fate: systematic devaluation. These roles center on presence, empathy, and human development, yet they are treated as cost centers rather than value drivers. Why? Because they resist commodification and do not scale into neat productivity metrics.
This pattern is gendered. Historically, caregiving and relational labor have been feminized, coded as “soft” work, and therefore underpaid and under-protected. Misogyny operates structurally here: the economy rewards extraction and speed, while discounting labor associated with nurturing, listening, and sustaining life. When markets dominate governance, anything aligned with traditionally feminine-coded values—care, teaching, emotional labor—becomes economically invisible.
Palliative care is the stress test because it collides head-on with this bias. Its core outputs—time, trust, moral containment—are intangible. They do not generate billable events at the same rate as procedures. The result: a specialty essential for dignity is treated as expendable. This is not an accident; it reflects a cultural hierarchy that prizes technical intervention over relational repair. Until policy and payment systems confront this bias, every promise of “patient-centered care” will remain hollow theater.
Fixing this requires more than resilience training. It demands structural change: payment models that reward relational outcomes, nonprofit accountability for mission fidelity, guardrails on extractive finance, and governance that restores clinician voice. Without these, every promise of “patient-centered care” is theater.
Going Deeper
Why does this happen? Because the system runs two operating systems: one speaks moral language, the other executes financial code. Marketization reframes care as a commodity. Corporatization concentrates power and erodes autonomy. Financialization invites private equity to treat hospitals like hedge funds. Each force pulls toward solvency, not solidarity.
Metrics are the gears. They privilege what scales—procedures, volumes—not what matters: presence, trust, and meaning-making. Relational outcomes vanish because they resist quantification. And when dashboards become doctrine, clinicians become widgets.
The result is structural moral injury. You are told you matter while being managed like a cost center. That mismatch destabilizes identity and drives distress. It’s not hypocrisy; it’s design.
1. Structural Drivers
Marketization, commercialization, corporatization, and financialization didn’t just “influence” healthcare—they rewired its DNA:
- Marketization reframed care as a commodity, replacing professional norms with price sensitivity.
- Commercialization normalized “no margin, no mission,” eroding nonmarket obligations.
- Corporatization concentrated power, subordinating clinician autonomy to scale and leverage.
- Financialization introduced private equity’s extractive logic, accelerating debt-driven cost pressures.
Tsang’s metaphor of the “abominable creature” complements this: the system is a Frankenstein assembled from individually rational choices—each merger, each reimbursement tweak, each benefit design—until the aggregate form is monstrous. The $4.9T flow map he presents is not chaos; it’s a kraken whose tentacles are incentive structures.
2. Pulverized Values
Both of these sources support my analysis that even the best intentioned, formulated, and messaged values are pulverized by operational layers between even the most visionary health system leaders and the folks on the ground. Blumenthal shows how nonmarket values (charity, professionalism) were displaced by market norms. Tsang illustrates the cumulative effect: decisions favoring treatment over prevention, innovation over affordability, old-age repair over childhood investment. These aren’t random—they reflect a system optimized for throughput and capital return, not relational care.
3. Palliative Care is the Canary
Blumenthal’s taxonomy explains why palliative care is maybe not doing so well in that coal mine:
- It resists commodification.
- Its outputs (meaning-making, legacy building, family and medical team dynamic assessments and interventions) are economically illegible.
- Under financialization, services without rapid, legible ROI are liabilities.
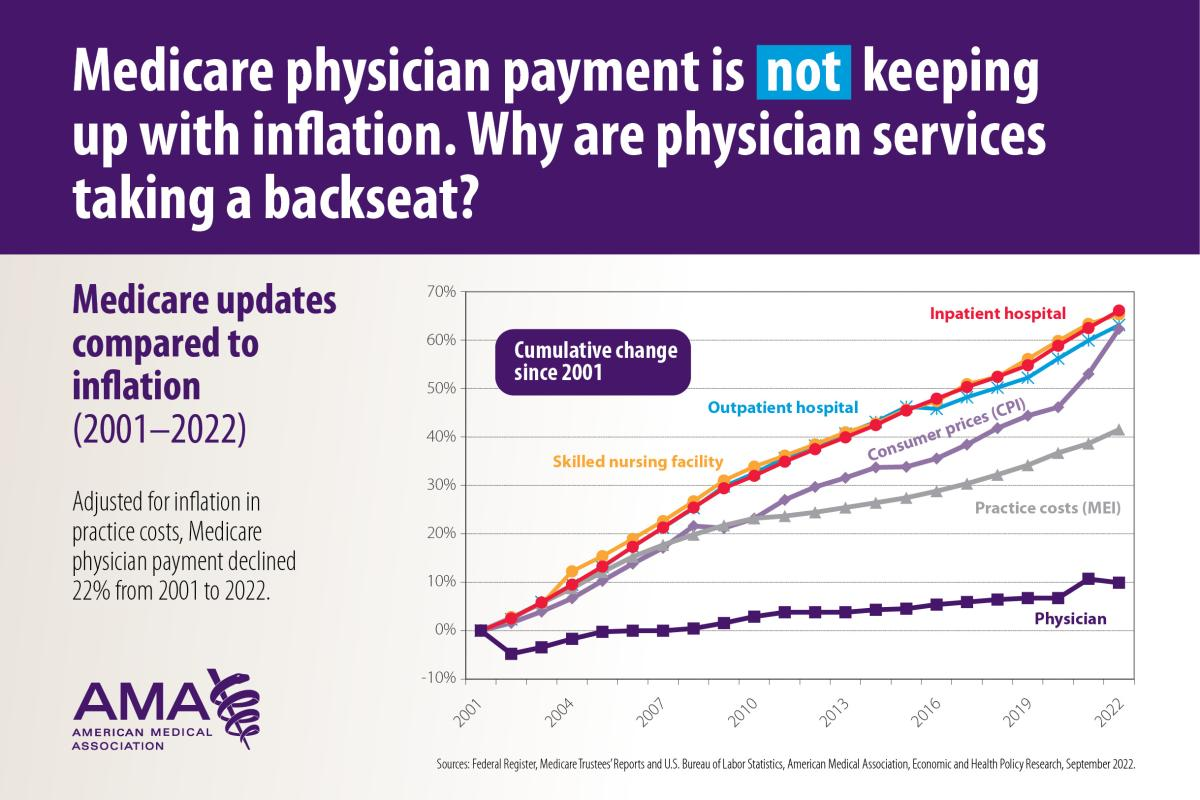
Tsang’s analysis sharpens this: the U.S. system allocates $1.5T to hospital care vs. $100B to public health. Hospice and home health are dwarfed by acute interventions. Hospitals have received ever-increasing reimbursement, yet whinge about paying for a few palliative care team members:
The abominable creature’s anatomy reveals priorities that make our work structurally precarious.
4. So Is this Gaslighting?
The harm we feel is systemic, (probably) not conspiratorial. “Gaslighting” captures the subjective experience—verbal affirmation paired with operational negation—but analytically, this is institutional betrayal.
Leaders inherit a machine whose operating system is financial logic. They speak moral language while executing code written for margin.
5. Moral Injury as Systemic Externality
Blumenthal warns that corporatization and financialization deprofessionalize clinicians unless countered by aligned incentives. Tsang’s kraken metaphor shows why this rarely happens: every tentacle pulls toward solvency, not solidarity. Compassion becomes an externality—essential for legitimacy, unfunded in practice.
Okay, But What Do We Do?
Local Level
- Balance Scorecards: Replace RVU-only dashboards with metrics that include time-in-conversation, goals-of-care documentation, and patient-reported experience.
- Clinician Governance: Create formal channels for clinician input and veto power on safety and relational care standards. And it's long past time for a national physician union.
- Guardrails on Incentives: Cap panel sizes, protect visit length for complex care, and decouple pay from pure productivity.
Regional / Organizational Level
- Mission Fidelity Audits: Tie executive bonuses to community health needs assessments (CHNA) and relational outcomes, not just margin.
- Transparency in Ownership: Require disclosure of private equity stakes and corporate roll-ups within health systems.
- Workforce Well-being Plans: Implement system-level strategies from the National Academy of Medicine, including administrative burden reduction and EHR workflow redesign.
State Level
- Nonprofit Accountability: Standardize definitions for community benefit spending and enforce reporting tied to CHNA priorities.
- Antitrust Enforcement: Monitor and limit excessive consolidation that erodes competition and clinician autonomy.
- Guardrails on Financial Practices: Restrict sale-leaseback arrangements and leveraged buyouts that destabilize care delivery.
Federal Level
- Payment Reform: Embed patient-reported outcome and experience measures (PROMs/PREMs) into ACOs, Medicare Advantage, and specialty bundles with staged incentives.
- Ownership Transparency Mandates: Require national reporting of private equity and corporate ownership structures.
- Regulatory Oversight: Close coding loopholes, strengthen corporate practice of medicine laws, and enforce surprise billing protections.
Remedies for Gendered Undervaluation
- Pay Equity Mandates: Enforce equal pay for roles dominated by relational labor, including palliative care, teaching, and social work.
- Relational Metrics in Reimbursement: Tie payment to documented time spent on communication, shared decision-making, and emotional support.
- Workforce Protections: Guarantee safe staffing ratios, predictable schedules, and benefits for relational roles to reduce burnout and attrition.
- Career Pathways and Prestige: Create leadership tracks and research funding for relational specialties to elevate status and influence.
Making Relational Work Appealing to Men
- Rebrand and Normalize: Market relational roles as high-skill, high-impact professions emphasizing complexity and leadership potential.
- Mentorship and Sponsorship: Develop male-inclusive mentorship programs and visible male champions in palliative care and similar fields.
- Compensation Transparency: Publicize competitive salaries and advancement opportunities to counter stereotypes of low pay.
- Education and Exposure: Integrate relational care rotations early in medical and professional training to normalize participation across genders.
Conclusion
The bottom line: the machine behaves as designed. To make compassion operational, redesign the incentives, protect the mission, and give clinicians authority where care decisions are made. Until then, expect more dashboards, more quotas, and more moral injury—because in this system, humanity is always out of stock.





