Death, Creativity, and Compassion: What Are We Really Training For?

In specialist palliative care, we talk about “compassion training” as if it’s a discrete skill you can add to a checklist. Joan Halifax’s enactive model challenges that notion: compassion isn’t a module; it emerges when attentional clarity, affective balance, ethical intention, and embodied engagement cohere in context.
Now, contrast that with the terror management literature: when death anxiety spikes, people don’t usually blossom into bodhisattvas. They double down on worldviews, punish norm violators, and cling to cultural scripts. Mortality salience makes us rigid. Death reflection—imagining the smoke-filled room, the scalding doorknob—might do something different. It forces a reckoning: What life have I lived? What matters now? That’s not defensive; that’s transformative.
Why This Matters
We say we teach compassion. But under pressure, what do we really train? Evidence from psychology suggests that when death anxiety spikes, people don’t open up—they clamp down. They cling to cultural scripts, punish norm violators, and chase self-esteem. That’s defense, not presence.
If compassion is what we want, we need to rethink our methods.
Mortality Salience vs. Death Reflection
Two ways to confront mortality:
- Mortality Salience: “Write about your own death.” Predictable result? Defensive rigidity.
- Death Reflection: “Imagine you have minutes left—what matters most?” This primes meaning-making and relational focus.
Question for us: Are our training exercises creating openness—or reinforcing defenses? Are those of us drawn to work in healthcare working through our own fears of death?
Compassion Isn’t a Module
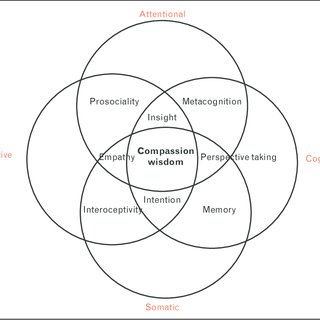
Joan Halifax’s work reframes compassion as an emergent process, not a checklist item. It arises when:
- Attention is steady.
- Emotions are regulated.
- Intention is ethical.
- Presence is embodied.
You don’t “teach compassion” in a slide deck. You create conditions for it to emerge—through mindfulness, perspective-taking, and embodied practice.
Terror Management Theory (TMT)
Carries the foundational premise that humans possess a self-preservation instinct and are uniquely aware of inevitable death, creating potential for paralyzing existential terror. In this model, mortality salience activates defenses to preserve self-esteem and cultural worldviews. In clinical settings, this may manifest as:
- Deflection and intellectualization (more on this in a minute)
- Moral outrage or avoidance when symbolic immortality feels threatened.
Poor communication may not just be a skill deficit—it could be an existential defense mechanism.
Solution: A dual-component cultural anxiety buffer.
- Cultural worldview: Provides meaning, order, and promise of literal or symbolic immortality.
- Self-esteem: Belief in living up to cultural standards of value.
This buffer allows pursuit of life goals without being overwhelmed by death anxiety.
Let's hit the down-button (thanks Sue Johnson) and go one floor deeper with a dual-process model:
- Proximal Defenses: Activated by conscious death thoughts; rational, threat-focused strategies (suppression, denial, health optimism).
- Distal Defenses: Activated by unconscious but accessible death thoughts; experiential, symbolic strategies (worldview defense, self-esteem bolstering).
Key Insight: Mortality salience effects occur without conscious anxiety; strongest when death thoughts are accessible but outside focal attention.
Creativity as an Existential Buffer
Sligte and colleagues show that death anxiety can choke originality—unless you give people a shot at legacy. And I'd argue that it's perhaps impossible to practice high-level palliative care without creativity! When creativity promises symbolic immortality, mortality salience flips from a cognitive straightjacket to a generative spark. But only if the culture values creativity. Only if the act connects to meaning.
Kyle's Working Schema:
- Death anxiety is a pivotal emotional driver influencing communication quality in medicine.
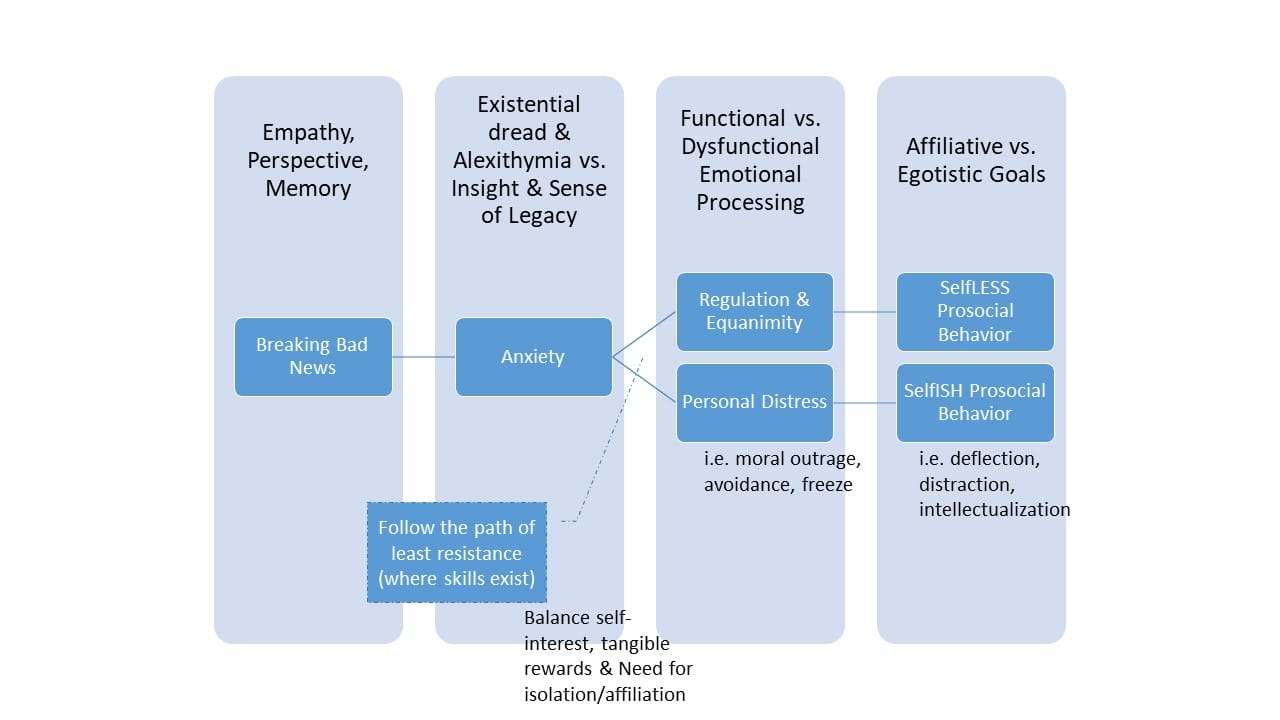
- Two contrasting pathways emerge:
- Suboptimal communication: Triggered by death anxiety + low symbolic immortality → avoidance, freeze, moral outrage, selfish prosocial behavior.
- Optimal communication: Death anxiety + high symbolic immortality → regulation, equanimity, selfless prosocial behavior, empathy, perspective-taking.
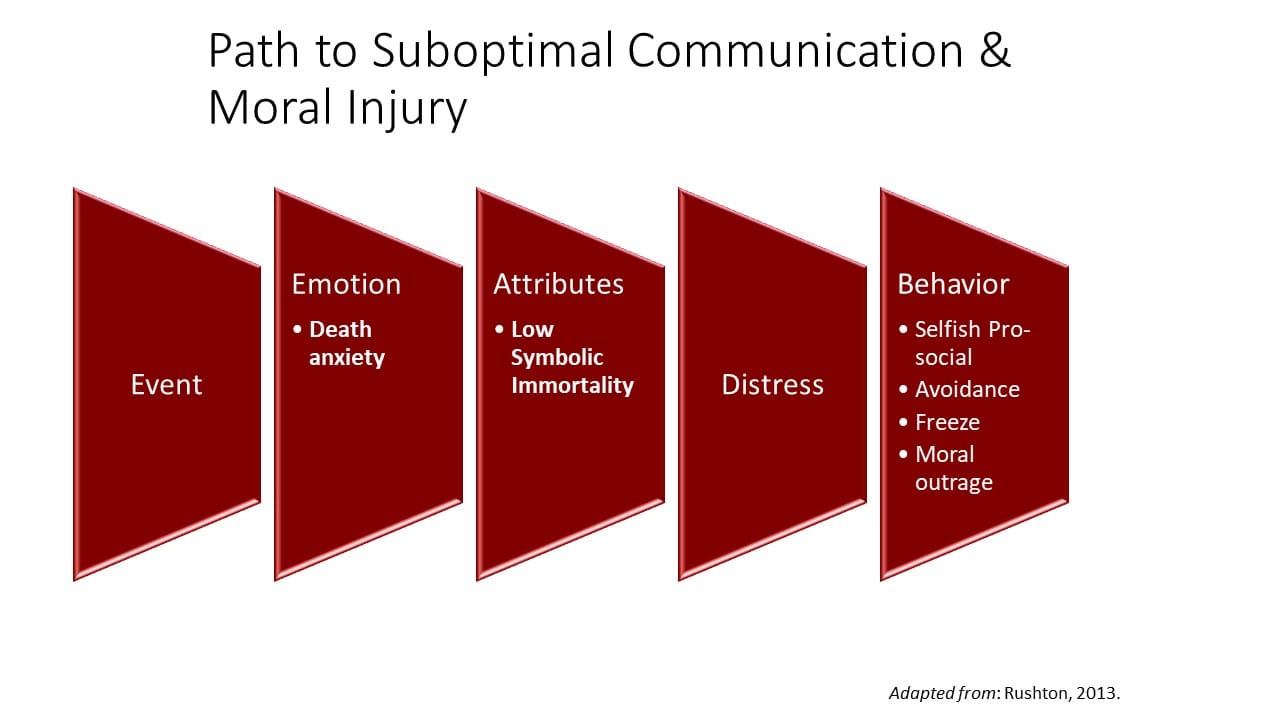
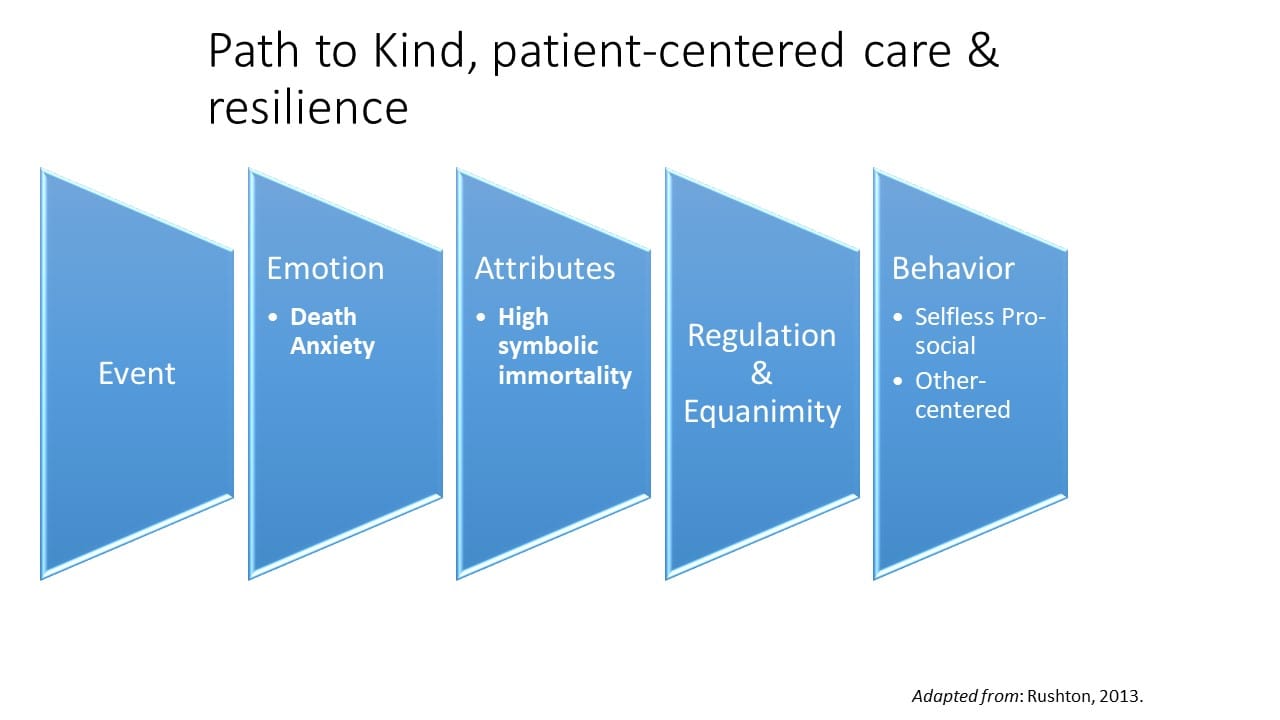
- Attributes like moral sensitivity, memory projections, and cognitive attunement are central to whether clinicians respond with compassion or defensiveness.
Practice Corner
Quick Experiments for You and Your Team
- Death Reflection Prompt
- "If this were your last week in medicine, what one thing would you change about your care today?"
- “Whose voice do you most need to hear on this case and why have you not heard it yet?"
- Micro Mindfulness 1-2-3
- Breath count to 10. Do this while you gel your hands.
- Name three body sensations without judgment.
- Repeat before hard conversations.
- Equanimity micro‑practice:
- Silently repeat “I will act compassionately; I cannot force outcomes.”
- Then ask a single perspective‑taking question: “What matters most today?”
- De‑escalation drill
- When anger or fear narrows attention, pause and widen sensory field—three sounds, three sights, one scent
- Then re‑engage with a question instead of a statement.
- Legacy of Care
- Write a 150-word “What we learned from this patient” note.
- Save it. Share it. Let it shape future care.
Are We Training Presence or Policing Worldviews?
TMT’s meta‑analysis shows mortality salience effects are robust across cultures and tasks. In high‑pressure hospitals, throughput targets, rigid protocols, and evaluative climates amplify defensive modes. Halifax’s model requires a different ecology: attentional stability, ethical humility, and embodied engagement.
If culture rewards compliance and performance under time stress while withholding time for reflection and interoception, we engineer defenses. If we want clinicians who can sit with terror without clamping down, we must redesign education, supervision, and daily routines accordingly.
Look Around You And Ask...
- Which elements of our environment promote proximal defenses (suppression, denial)? Which promote distal defenses (worldview policing)?
- Which promote enaction (presence, discernment, readiness to act)?
- Where can we swap mortality salience‑style exposure for death reflection‑style mindfulness without losing efficiency?
- What one legacy‑building practice could we implement this month that is socially valued by our team and endures?
TL;DR in Rant Form
In palliative care, we preach presence and compassion, but our systems reward throughput and compliance. Are we training clinicians for attentional balance and ethical humility—or for worldview defense in a white coat? When we talk about “resilience,” do we mean equanimity or a corrosive immortality project—defending reputations, accumulating metrics, curating our own narratives of the “good death”? When our need for symbolic immortality collides with a patient’s need for presence, whose agenda wins? Are we willing to loosen our grip on outcomes, as Halifax urges, or are we still scripting rituals to soothe our own anxiety?
And here’s what I wrestle with:
- If death anxiety drives rigidity, and compassion requires openness, how do we design environments that tilt toward emergence rather than defense?
- Should we be integrating death reflection exercises—not just mindfulness—into clinician training?
- Could fostering creativity in care teams (legacy projects, narrative medicine) serve as an existential buffer that’s healthier than conformity?
- Finally, what happens when our own need for symbolic immortality collides with the patient’s need for presence? Are we willing to let go of the outcome, as Halifax urges, or are we still trying to script a “good death” to soothe our own terror?
If you’re feeling uncomfortable, me too. That’s the point. Comfort is the enemy of growth—and maybe of compassion.





