Precision Symptom Management: Why Palliative Care Is Poised for a Genomic Revolution

The News That Sparked This Post
Tempus AI’s acquisition of OneOme’s pharmacogenomics (PGx) assets is making headlines in precision medicine circles. Most observers see this as an oncology play. They’re not wrong—Tempus has built its reputation on molecular oncology and AI-driven insights. But here’s the bigger picture: this move could catalyze a transformation in how we manage pain and symptoms for patients with serious illness. And that’s a frontier we’ve ignored for far too long.
OneOme, a Mayo Clinic spin-off, was a recognized leader in PGx testing, offering its 27-gene RightMed panel to guide medication choices. Despite financial struggles that led to its closure, OneOme had partnerships with dozens of health systems and international reach. Tempus’ acquisition isn’t just about technology—it’s about relationships and market access. That matters because PGx is poised to move beyond oncology into broader clinical domains, including palliative care.
“This move could catalyze a transformation in how we manage pain and symptoms for patients with serious illness.”
The Untapped Frontier
Palliative care serves over 6 million patients annually in the U.S., yet pain management remains stuck in a trial-and-error paradigm. Opioid prescribing is fraught with variability, adverse effects, and risk. We know the genes—CYP2D6, CYP3A4, OPRM1—shape opioid metabolism and response. We know PGx can guide antidepressants and anticonvulsants used as adjuvants. So why are we still guessing?
The U.S. palliative care market is projected to grow from $1.15 billion in 2025 to $2.51 billion by 2035, driven by an aging population and rising prevalence of chronic illness. Yet innovation in this space has lagged behind oncology and cardiology. Precision symptom management—using genomics and AI to tailor interventions—offers a way to close that gap.
“Precision symptom management isn’t science fiction—it’s a moral imperative.”
What Precision Pain Management Looks Like
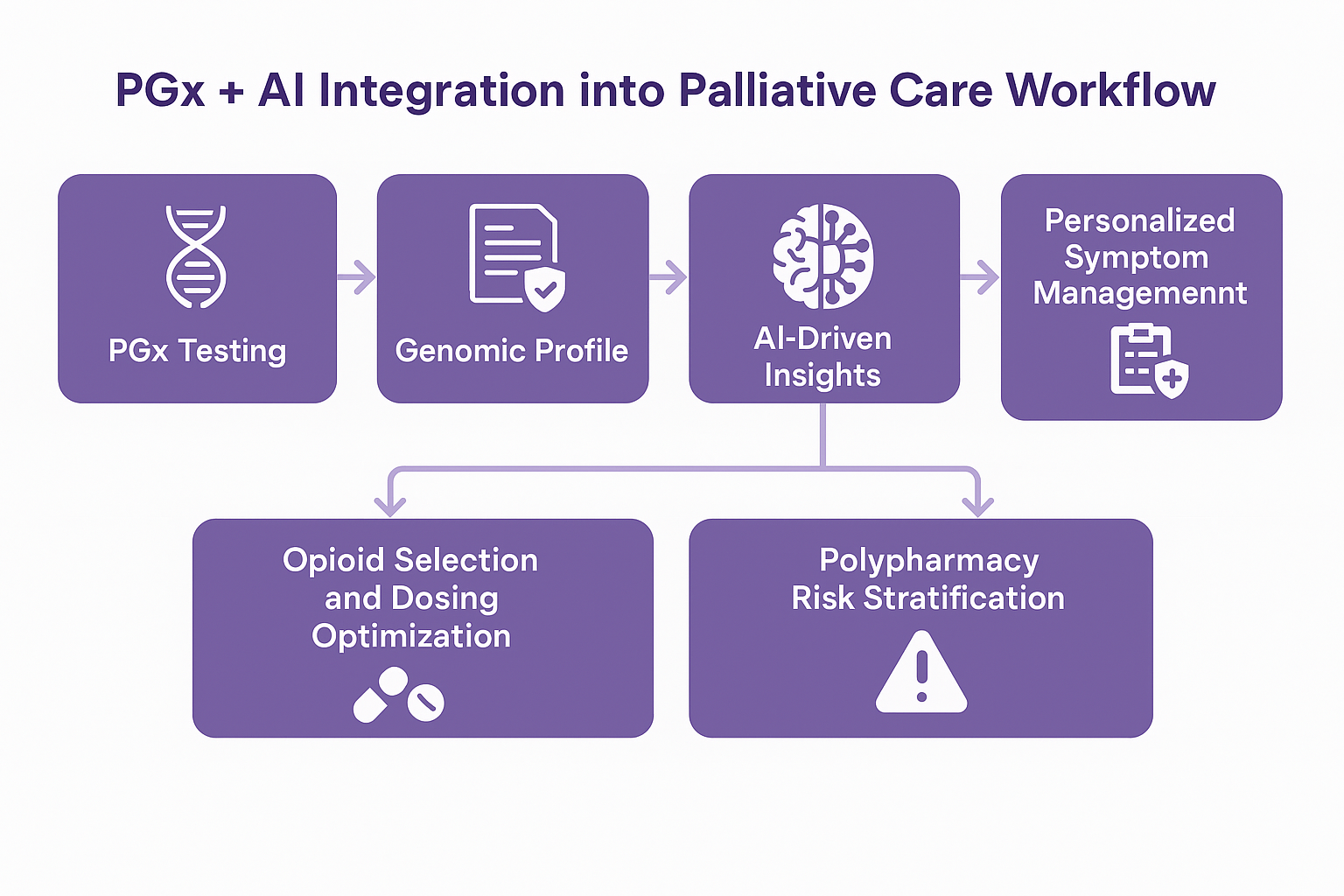
Imagine a workflow where:
- A patient’s PGx profile informs opioid selection and dosing.
- AI predicts symptom trajectories and flags high-risk polypharmacy.
- Clinicians move from reactive prescribing to proactive, personalized care.
PGx-guided opioid prescribing is already supported by Clinical Pharmacogenetics Implementation Consortium (CPIC) guidelines, which recommend tailoring codeine, tramadol, and hydrocodone therapy based on CYP2D6 phenotype. Research shows that poor metabolizers of CYP2D6 experience inadequate pain control and higher rates of emergency visits for pain management. Integrating these insights into palliative workflows could reduce suffering and prevent harm.
Why Now?
Tempus has the infrastructure: data platforms, AI capabilities, and now OneOme’s PGx expertise. Extending these tools beyond oncology into palliative care isn’t just good strategy—it’s good medicine. The company’s recent acquisitions of Ambry Genetics and Deep 6 AI underscore its ambition to expand into multi-disease precision care and leverage AI for clinical decision support.
Meanwhile, the evidence base for PGx in pain management is growing. Studies highlight that 14% of patients carry high-risk genotypes for opioid metabolism, and nearly half have intermediate-risk profiles requiring dose adjustments or alternative therapies. Yet adoption remains limited, often due to operational barriers and lack of clinician familiarity.
The Stakes
- Clinical: Reduce opioid-related harm, improve symptom control, and minimize adverse drug reactions.
- Economic: Chronic pain costs the U.S. $635 billion annually in healthcare expenses and lost productivity. PGx-informed prescribing could lower costs by reducing ED visits and hospitalizations.
- Human: Restore dignity and comfort at life’s most vulnerable moments.
Ethical Dimensions
Precision medicine in end-of-life care raises profound ethical questions. AI-driven decision support and genomic profiling must complement—not replace—the “warm touch” of palliative care. Risks include algorithmic bias, privacy concerns, and the potential for depersonalization if patients are reduced to data points.
Ethical frameworks emphasize:
- Transparency: Patients and families must understand how genomic and AI tools inform care.
- Equity: Avoid widening disparities in access to advanced technologies.
- Humanization: Technology should enhance, not erode, relational aspects of care.
As one review notes, maintaining “high-touch in high-tech” environments is essential to preserve dignity and trust at the end of life.
“High-touch in high-tech environments is essential to preserve dignity and trust.”
Barriers and Opportunities
Challenges include:
- Limited clinician training in PGx interpretation.
- Integration into electronic health records and workflows.
- Reimbursement uncertainties.
Opportunities:
- Embedding PGx alerts into prescribing systems.
- Leveraging AI for predictive symptom modeling.
- Building interdisciplinary advisory boards to guide implementation.
Call to Action
Precision symptom management is the next frontier. If you’re working at the intersection of genomics, AI, and patient comfort, let’s talk. The future of palliative care is data-driven—and it starts now.





